


Sinusitis is a common condition caused by inflammation, with or without infection, of one or more paranasal sinuses (the air-filled cavities in the bones of the skull).
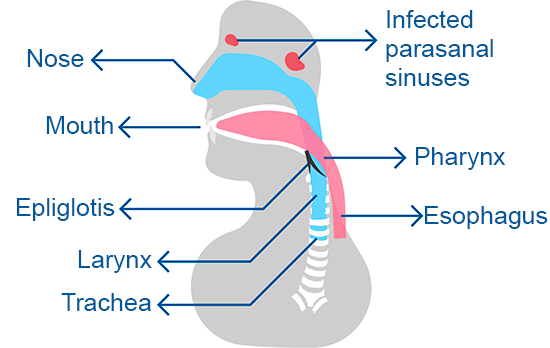
The primary cause of sinusitis is the blockage of sinus openings.
This obstruction reduces blood circulation and air entry into the sinus cavity, preventing proper mucus clearance and leading to lower oxygen levels. These conditions create an environment that promotes bacterial growth and infection.
Acute sinusitis is often preceded by a viral infection of the upper respiratory tract (commonly a cold). In some cases, infection does not occur, such as in:
In most cases, sinusitis involves an infection, which can be acute or chronic. The most common causes are:
Other factors associated with sinusitis include:
The most common symptoms of acute sinusitis (sudden onset with a duration of less than ten days) include:
Patients with chronic sinusitis (lasting more than 12 weeks or three months) typically experience:
In some cases, patients with chronic sinusitis may have no noticeable symptoms.
In children with chronic sinusitis, cough is the most common complaint, while fever is less frequent.
A thorough medical history and physical examination are essential and can identify purulent sinusitis in approximately 80% of cases.
During the clinical examination of acute sinusitis, typical findings include red and inflamed nasal mucosa, purulent nasal discharge and sinus tenderness when pressure is applied.
In cases of chronic sinusitis, the physical examination may appear normal or reveal nasal polyps or persistent purulent nasal discharge.
Radiography and computed tomography (CT) of the paranasal sinuses are generally not useful for diagnosing acute sinusitis. These tests are reserved for cases with diagnostic uncertainty and sinusitis unresponsive to antibiotics.
CT scans are particularly valuable for visualizing the contents and bony anatomy of the sinuses, especially in severe cases, such as suspected sphenoid or ethmoid sinusitis, or when tumors are a concern.
For patients with recurrent sinusitis, it is important to consider both allergic and non-allergic factors. Diagnostic tools include allergy skin testing, immunoglobulin testing, sweat chloride testing (to assess for cystic fibrosis) and ciliary motility studies.
In some cases, an otolaryngologist may perform a nasal endoscopy (rhinoscopy) to assess the nasal passages and identify the cause of obstruction.
The treatment of sinusitis focuses on eliminating the infection (if present) and restoring proper drainage of the paranasal sinuses.
Acute sinusitis can often resolve completely, while chronic sinusitis is more challenging to manage and control.
Most cases of acute sinusitis are viral and do not require antibiotics. However, distinguishing between viral and bacterial sinusitis can be difficult, as both share similar symptoms.
Initial treatment may involve nasal irrigation (saline nasal washes) and decongestants, with observation for spontaneous improvement. Bacterial sinusitis, though less common, can lead to serious complications. Therefore, it is important to monitor for signs of worsening.
Antibiotics may be necessary if symptoms persist for more than 10 days and include nasal congestion, mucopurulent discharge, and facial pain. They are also indicated if symptoms worsen rapidly, especially if there is severe facial or headache pain.
The choice and dosage of antibiotics should be determined by a healthcare provider after careful evaluation of each case.
Patients must follow medication instructions precisely to avoid complications. The duration of treatment is typically 10 to 14 days for acute sinusitis and 3 to 4 weeks for chronic sinusitis.
Decongestants and corticosteroids may be prescribed in specific cases, with clear instructions for their use.
If symptoms do not improve, a sinus lavage performed by an otolaryngologist may be required.
Surgery may be considered in cases of:
Surgical intervention must be followed by medical treatment, which may include various medications specific to the patient’s needs.
With the widespread use of antibiotics, serious complications of sinusitis are now rare. However, some potential complications include:
Acute ethmoidal sinusitis is more common in children than in adults and can lead to unilateral orbital and periorbital swelling or Periorbital cellulitis (severe inflammation around the eye).
Show more