How else can it be called?
Adenocarcinoma of the endometrium
Endometrial adenocarcinoma
Uterine corpus cancer
ICD-10: C54.1
What is endometrial cancer?
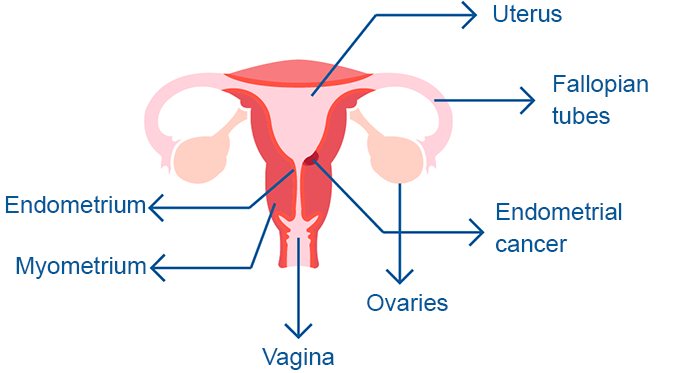
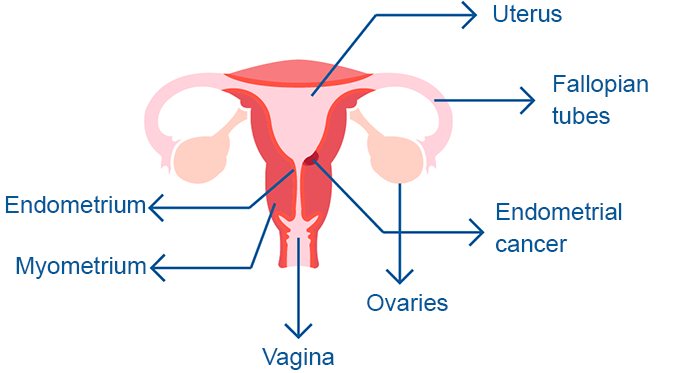
Endometrial cancer is a common type of cancer in women, typically occurring in those over the age of 45. It involves the development of cancerous (malignant) cells in the inner lining (endometrium) of the uterus.
The uterus is a hollow, inverted pear-shaped organ where a fetus develops during pregnancy.
Endometrial cancer is distinct from cervical cancer and cancers of the uterine muscle, such as uterine sarcoma or leiomyosarcoma.
Three layers can be identified in the body of the uterus:
- Endometrium: The inner layer of the uterus. During each menstrual cycle, the endometrium thickens, degrades, and ultimately sheds, resulting in menstrual bleeding.
- Myometrium: The intermediate muscular layer. This flexible muscular layer facilitates uterine contractions during childbirth. It is the layer where sarcomas typically originate.
- Perimetrium: A very thin, external serous layer (derived from the peritoneum) that covers the outer surface of the uterus.
What are the different types of endometrial cancer?
Endometrial cancer originates in the inner lining of the uterus and is the most common type of uterine cancer.
Based on the affected cells and their appearance under a microscope, the most common types of endometrial cancer include:
- Adenocarcinoma
- Endometrial carcinosarcoma
- Primary squamous cell carcinoma
- Small-cell carcinoma
- Transition cell carcinoma
- Serous carcinoma
Identifying the type of cancer is crucial because it helps predict the tumor's behavior and guides the development of a specific treatment plan.
How many people does it affect?
Endometrial cancer primarily affects postmenopausal women, typically those over 60 years of age.
Globally, endometrial cancer is the 7th most common type of cancer among women.
What are the risk factors for endometrial cancer?
The primary risk factor for endometrial cancer is elevated levels of estrogen (a female sex hormone). These high levels can occur naturally in the body or result from medication use.
Other risk factors include:
- Early menstruation (before age 12) or late menopause.
- Family history of endometrial or related cancers.
- Never having been pregnant.
- Infrequent menstrual cycles.
- Obesity.
- Polycystic ovary syndrome (PCOS).
- History of endometrial polyps.
- Ovarian cancer.
- Lynch syndrome.
- Cowden syndrome.
- Mutations in the BRCA1 or BRCA2 genes.
What are the symptoms of uterine endometrial cancer?
Like most cancers, endometrial cancer is most effectively treated when detected early. Initial symptoms may include:
- Unusual bleeding or discharge not related to menstruation (metrorrhagia).
- Lower abdominal pain.
- Purulent (pus-like) vaginal discharge.
- Difficulty or pain during urination.
- Pain during intercourse (dyspareunia).
- Pelvic pain.
Additionally, endometrial cancer has been observed in some breast cancer patients who were treated with the hormone tamoxifen.
How can it be detected?
The main tests to detect endometrial cancer are:
- Pelvic Examination: During the exam, the doctor palpates the pelvic area to look for masses or changes in the shape of the uterus.
- Papanicolaou (Pap) Test: Primarily used to screen for cervical cancer, the Pap test involves using a cotton swab, a cytobrush, and a wooden spatula to gently scrape cells from the cervix (the opening of the uterus) and the vagina. While its main purpose is to detect cervical abnormalities, it can sometimes identify abnormal endometrial cells.
- Ultrasound or Transvaginal Ultrasound: These imaging techniques allow doctors to visualize the uterus, identify tumor lesions, and determine their size and location.
- Hysteroscopy: This procedure involves inserting a thin, flexible tube with a camera (hysteroscope) through the cervix to visually examine the interior of the uterus. It allows for direct observation and the collection of biopsy samples.
- Endometrial Aspiration Biopsy.
The prognosis (chance of recovery) and selection of treatment depend on the stage of the cancer—whether it is confined to the endometrium or has spread to other parts of the uterus or the body—as well as the patient's overall health.
To determine the extent of cancer involvement and to plan appropriate treatment, further imaging studies may be performed, including:
- Abdominal ultrasound.
- Chest CT scan.
- Magnetic resonance imaging (MRI) of the abdomen and pelvis.
- PET scan (Positron Emission Tomography).
What are the stages of cancer?
Endometrial cancer is classified into the following stages:
- Stage I. The cancer is confined to the main body of the uterus and has not invaded the tissues of the cervix.
- Stage II. Cancer cells have spread to the cervix but remain within the uterus.
- Stage III. The cancer has spread beyond the uterus but is still confined to the pelvic area.
- Stage IV. Cancer cells have spread outside the pelvis to other parts of the body, such as the bladder, rectum, or distant organs.
- Recurrent. Recurrent disease refers to cancer that has returned after treatment. It may recur in the uterus, pelvis, or other parts of the body.
What is the recommended treatment?
When endometrial cancer is detected early, it typically has a favorable prognosis and is often curable.
Treatment options depend on the stage of the cancer—whether it is confined to the endometrium, involves the rest of the uterus, or has spread to other parts of the body.
Various treatments may be used:
- Surgery (removal of the uterus).
- Radiotherapy (Uses high-energy radiation to kill cancer cells):
- External radiation therapy: Delivers radiation from outside the body to the cancerous area.
- Internal radiotherapy: Places radioactive materials (e.g., needles, wires, or catheters) directly inside or near the cancer.
- Chemotherapy: Uses drugs to kill cancer cells, often referred to as "poisons".
- Targeted Therapy: Employs drugs that identify and attack specific cancer cells:
- Monoclonal antibodies.
- mTOR inhibitors.
- Signal transduction inhibitors.
- Immunotherapy.
- Hormone Therapy (Uses hormones or hormone-blocking agents to slow or stop the growth of certain types of endometrial cancer.).
Surgery is the most common treatment for endometrial. The cancer is typically removed through a hysterectomy, a procedure in which the entire uterus and fallopian tubes are removed, or, in some cases, the uterus along with the fallopian tubes and ovaries (salpingo-oophorectomy).
- Abdominal hysterectomy: The uterus is removed through an incision in the abdomen (similar to a cesarean section or laparoscopy).
- Radical hysterectomy: Involves removing the uterus, cervix, part of the vagina, and lymph nodes in the area.
- Tumor cytoreduction: In advanced cases, as much of the tumor as possible is removed. This may involve removing the uterus, cervix, fallopian tubes, ovaries, vaginal dome, and part of the peritoneum (a serous layer where metastases may occur).
What are the recommended treatments at each stage?
Treatments for endometrial cancer depend on the stage of the disease, the size of the tumor, the patient's age, and general health.
- Stage I. Treatment may include:
- Total abdominal hysterectomy with bilateral salpingo-oophorectomy and lymph node dissection. Post-surgery radiotherapy and/or chemotherapy.
- Radiotherapy alone for selected patients.
- Stage II. Treatment may include:
- Total abdominal hysterectomy with bilateral salpingo-oophorectomy and lymph node dissection, followed by post-surgery radiotherapy.
- Radiotherapy, followed by total abdominal hysterectomy with bilateral salpingo-oophorectomy and lymph node dissection.
- Radical hysterectomy.
- Stage III. Treatment may include:
- Radical hysterectomy, usually followed by radiotherapy.
- Local radiotherapy alone.
- Hormonal therapy.
- Immunotherapy.
- Targeted therapy.
- Stage IV: Treatment may include:
- Radiotherapy.
- Hormonal therapy.
- Chemotherapy (including clinical trials).
- Adjuvant therapy (additional treatments to complement the primary treatment).
- Cytoreduction surgery (removal of as much of the tumor as possible).
- Immunotherapy.
- Targeted therapy.
- Recurrences: Treatment of recurrence may include:
- Radiation therapy to relieve symptoms like pain, nausea, and abnormal bowel function.
- Hormonal therapy.
- Chemotherapy (including clinical trials).
- Targeted therapy.
Bibliography
- Cancer Epidemiology and Prevention (4th Ed), Linda S. Cook, Angela L. W. Meisner, and Noel S. Weiss, ISBN: 978-0-1902-3866-7, Pag. 909.
- Robbins Basic Pathology (10th Ed) 2018, Vinay Kumar, Abul K. Abbas, Jon C. Aster, ISBN: 978-0-323-35317-5, Pag. 724.
- Endometrial Cancer. Cancer.org. American Cancer Society. Available on: https://www.cancer.org
- Endometrial Cancer. Mayo Clinic. Available on: https://www.mayoclinic.org
- Volume155, IssueS1 Special Issue: FIGO Cancer Report 2021 October 2021.
- SEOM-GEICO clinical guidelines on endometrial cancer (2021). Sociedad española de Oncología médica. Available on: https://seom.org
Show more
Rating Overview
Share your thoughts about this content