How else can it be called?
Cancer of the cervix
Cervical carcinoma
Uterine cervical cancer
ICD-10: C53
What is cervical cancer?
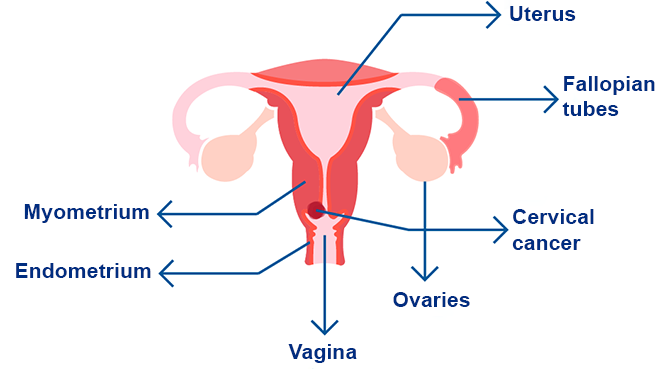
Cervical cancer is one of the most common types of cancer in women, characterized by the presence of malignant (cancerous) cells in the tissues of the cervix.
The uterus is a hollow, inverted pear-shaped organ where the fetus develops during pregnancy. The cervix, located at the lower part of the uterus, is an opening that connects the uterus to the vagina (birth canal).
This type of cancer begins with abnormal changes in the cells of the cervical epithelium (the surface tissue of the cervix). Over time, these cells can mutate and become cancerous, a process that may take years. Before cancer develops, normal cells often go through a premalignant phase called dysplasia, where cellular alterations can be detected through tests such as vaginal cytology or a Pap smear.
If untreated, the cancer cells may grow, spread, and infiltrate deeper into the cervix, and spread to nearby or distant organs, a process known as metastasis.
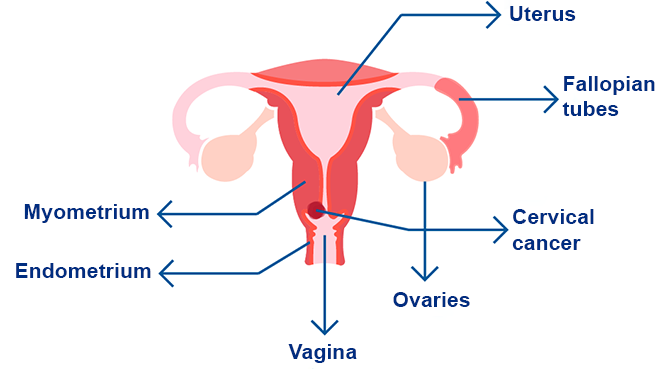
How is the cervix formed?
The cervix can be divided into two parts, each lined with different types of cells:
- Endocervix: This is the portion closest to the uterus, lined with glandular cells.
- Exocervix: This is the portion closest to the vagina, visible during colposcopy or Pap smear procedures. It is lined with squamous cells, also known as stratified squamous epithelium.
The area where these two parts meets is called the transformation zone, where the two types of cells coexist. The location of the transformation zone changes over time due to factors such as age and childbirth.
What is the origin of cervical cancer?
Cervical cancer originates in the transformation zone. This is where the endocervix and exocervix meet, and the stratified squamous epithelium of the exocervix transitions to the simple glandular columnar epithelium of the endocervix.
This area is particularly vulnerable to changes caused by microorganisms, such as the human papillomavirus (HPV), as well as physical or chemical agents like tobacco. These factors can induce cellular changes and mutations, leading to a condition known as dysplasia, which may eventually develop into cervical cancer.
What are the risk factors for cervical cancer?
Nearly all cervical cancers are caused by the human papillomavirus (HPV), which is primarily spread through sexual contact. There are more than 150 types of HPV, but 12 are considered high-risk or carcinogenic. These include the following genotypes: 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, and 59.
Other HPV types can cause common warts or genital warts, but they are not linked to cervical cancer.
Additional risk factors for cervical cancer include:
What are the most common types of cervical cancer?
The most common types of cervical cancer are:
- Squamous cell carcinoma: Accounts for about 90% of cases. It develops in the transformation zone from the squamous cells of the exocervix.
- Adenocarcinoma: Arises from the glandular cells of the endocervix.
Less common types include:
- Adenosquamous carcinoma (mixed carcinoma): Contains features of both squamous cell carcinoma and adenocarcinoma.
- Melanoma, sarcoma, or lymphoma: Rare types of cervical cancer.
Identifying the type of cancer is crucial, as it directly influences both prognosis and treatment.
What are the symptoms and signs of cervical cancer?
Cervical cancer often does not cause symptoms in its early stages.
As the cancer progresses, the following symptoms may appear:
- Metrorrhagia or intermenstrual bleeding: Abnormal vaginal bleeding that occurs between normal menstrual cycles.
- Watery vaginal discharge: May have a strong odor or contain traces of blood.
- Pelvic pain or dyspareunia: Pain during sexual intercourse.
How can it be detected?
Cervical cancer often does not cause symptoms in its early stages, so a series of tests are typically necessary for diagnosis:
- Cervical cytology (Pap smear or Papanicolaou test): This test is performed during a speculoscopy or colposcopy procedure, which allows the doctor to visualize the vaginal canal and cervix. Using a cotton swab, brush (cytobrush), or small wooden spatula, the doctor gently scrapes cells from the cervix (including the exocervix and the outer part of the endocervix) to collect a sample. The procedure may cause mild pressure or discomfort, and in some cases, slight pain. The collected sample is stained with special dyes (e.g., Harris hematoxylin and eosin) and examined under a microscope to detect abnormalities or microorganisms.
- HPV test: This test detects the presence of high-risk types of the human papillomavirus (HPV), which can cause cell changes leading to cervical cancer.
- Biopsy: If abnormal cells are found, a biopsy may be necessary. A tissue sample is taken from the cervix and analyzed under a microscope to confirm the presence of cancer cells. Types of biopsies include:
- LEEP (Loop Electrosurgical Excision Procedure): Uses a thin wire loop to remove a superficial portion of cervical tissue.
- Conization: Removes a cone-shaped portion of deeper cervical tissue for more detailed examination.
The prognosis (chances of recovery) and choice of treatment depend on the stage of the cancer (localized or metastatic) and the patient’s overall health.
Once a diagnosis is made, additional tests are used to determine the stage of the cancer and evaluate its spread. Transvaginal and abdominal ultrasounds, chest X-rays, and CT scans of the abdomen and chest help assess whether the tumor is confined to the cervix or has metastasized to other organs.
What are the stages?
To determine the stage of cervical cancer, a physical examination, imaging studies, and possibly biopsies are required. The stages are classified as follows:
Stage I: Cancer is confined to the cervix and has not spread to other parts of the body. It is further divided into:
- Stage IA: Diagnosed only by microscopic examination.
- Stage IA1: Cancerous area is less than 3 mm deep.
- Stage IA2: Cancerous area is 3 to 5 mm deep.
- Stage IB: Tumor is larger but still confined to the cervix.
- Stage IB1: Tumor measures more than 5 mm deep and less than 2 cm wide.
- Stage IB2: Tumor measures more than 2 cm deep and less than 4 cm wide.
- Stage IB3: Tumor is more than 4 cm wide.
Stage II: Cancer has spread beyond the cervix to nearby areas (such as the uterus or vagina) but remains within the pelvic region:
- Stage IIA: Tumor is confined to the upper two-thirds of the vagina and does not involve the parametrial region:
- Stage IIA1: Tumor is less than 4 cm wide.
- Stage IIA2: Tumor is more than 4 cm wide.
- Stage IIB: Tumor has spread to the parametrial region but not to the pelvic wall.
Stage III: Cancer has extended to the lower third of the vagina, the pelvic wall, or affects the kidneys, but there is no distant spread:
- Stage IIIA: Tumor involves the lower third of the vagina but not the pelvic wall.
- Stage IIIB: Tumor has reached the pelvic wall and/or affects kidney function.
- Stage IIIC: Tumor has spread to regional lymph nodes.
- Stage IIIC1: Cancer involves pelvic lymph nodes.
- Stage IIIC2: Cancer involves para-aortic lymph nodes.
Stage IV: Cancer has spread to distant parts of the body:
- Stage IVA: Cancer has invaded nearby organs, such as the bladder or rectum, but has not spread to distant areas.
- Stage IVB: Cancer has metastasized to distant organs, such as the lungs.
Recurrent cervical cancer. Recurrent disease means that the cancer has returned after treatment. It may reappear in the cervix or metastasize to another part of the body.
What is the treatment for cervical cancer?
There are various treatment options available for all patients with cervical cancer, depending on the stage and specific characteristics of the cancer. These treatments include:
- Surgery: Removal of cancerous tissue through an operation.
- Radiotherapy: Use of high-energy radiation to destroy cancer cells.
- Sentinel lymph node biopsy: During surgery, lymph nodes in the pelvis that are most likely to contain cancer are removed to check for cancer spread.
- Immunotherapy: Medications that stimulate the immune system to recognize and attack cancer cells.
- Targeted therapy: Drugs that target specific proteins involved in cancer growth. For example:
- Bevacizumab: Currently used to treat advanced cervical cancer.
- Cediranib and nintedanib: Other drugs under investigation for advanced cases.
- Chemotherapy: Drugs used to kill cancer cells.
Treatment decisions are based on factors such as the tumor's size, spread, and involvement with surrounding tissues and lymph nodes. In some cases, surgery options include:
- Cryosurgery: Removal of cancer by freezing the tissue.
- Laser surgery: Use of an intense beam of light to kill cancer cells.
- Conization: Removal of a cone-shaped piece of tissue from the cervix. This is often used for biopsies and early-stage cervical cancer treatment.
- Electrosurgical excision (LEEP): Uses an electric current passed through a thin wire loop to excise abnormal tissue.
- Hysterectomy: Removal of the uterus and cervix, as well as cancerous tissue.
- Vaginal hysterectomy: Removal of the uterus through the vagina.
- Abdominal hysterectomy: Removal of the uterus through an incision in the abdomen. It may also involve removal of the ovaries and fallopian tubes (bilateral salpingo-oophorectomy).
- Radical hysterectomy: Removal of the cervix, uterus, and part of the vagina, along with lymph nodes in the area.
- Pelvic exenteration: If cancer has spread beyond the cervix or female organs, it may be necessary to remove the lower colon, rectum, or bladder, along with the cervix, uterus, and vagina. This procedure may require reconstructive surgery, such as vaginoplasty, to create an artificial vagina.
Bibliography
- Cancer Epidemiology and Prevention (4th Ed), Rolando Herrero and Raul Murillo, ISBN: 978-0-1902-3866-7, Pag. 925.
- Bhatla N, et al. Revised FIGO staging for carcinoma of the cervix uteri. Int J Gynecol Obstet 2019; 1–7.
- International journal of Gynecology&Obstetrics. Cancer of the cervix uteri: 2021 update. Neerja Bhatla, Daisuke Aoki, Daya Nand Sharma, Rengaswamy Sankaranarayanan. FIGO CANCER REPORT 2021. Available on: https://doi.org
- If you have cervical cancer. American Cancer Society. Available on: https://www.cancer.org
- Cervical cancer. Mayo Clinic. Available on: https://www.mayoclinic.org
Show more
Rating Overview
Share your thoughts about this content